| Introduction | My Story | My Labs | My Meds | My Advice |
My Story
Ibuprofen or Scotch Spring, 1994 As I mentioned in the introduction, I started having joint pain in the Spring of 1994. I had been on a field test at Redstone Arsenal in Alabama and we were reducing data in a "facility" called the "White House," so named because it was a little, old, white house. The furniture and computer configuration were as un-ergonomic as one could find. I attributed the joint pain in my fingers to contortionist typing. When the pain didn't go away after I got back to my normal workstation, I went to see my internist, Dr. Tate. The blood work was normal and the migrating joint pain was my only symptom. Ibuprofen or Scotch were his suggestions, with Scotch being his preferred choice. And if this "migratory polyarthralgia" didn't go away, I was to come back in six to eight weeks. Six to eight weeks after my first visit, Dr. Tate repeated the blood work and this time the Anti-Nuclear-Antibodies (ANA) came back positive. With that, he referred me to a local rheumatologist, Dr. R. Michael Roberts.
3/4 of a Diagnosis Dr. Roberts ran some additional tests including an Anti-DNA (aDNA) titer, which came back positive. So with the joint pain, positive ANA, and positive aDNA, I had three of the eleven diagnostic criteria for Lupus. In general, a firm diagnosis of Lupus can be made when a person has exhibited four of the eleven criteria. So I was well on my way to a solid diagnosis of Systemic Lupus Erythematosis.
Pop the Finger The joint problems were odd. Sometimes I'd have swelling without pain, pain without swelling, or pain and swelling. Sometimes I'd blow on a puffy finger like I was inflating a balloon and hold it up and say, "Hey, look at this!" At the time, Lupus was an annoyance to me. I used lots of ibuprofen to try to manage the pain with limited success. I stopped flying kites because of the pain in my hands and the recommendation to avoid sun exposure. And I thought Lupus sucked back then.... Little did I know....
Zzzzzzzz..... By the end of the summer, I was becoming more and more exhausted. I'd go to bed early but when the alarm would go off at at 7:30 or so, I'd wake up and still be so incredibly tired that I'd roll over and sleep for another hour or two. Luckily my employer is fairly flexible and I was able to work a little later to make up the time. I tend to think of the difference between tiredness and fatigue as the difference between not feeling like getting out of bed and not being able to get out of bed. About this time, Dr. Roberts noticed I was becoming anemic. My hemoglobins were falling pretty steadily, giving me my fourth Diagnostic Criterion. So I started on 10mg of Prednisone and was referred to Dr. Harvey Rothberg, a hematologist.
High Point of the Day Dr. Rothberg explained that I could be anemic for a variety of reasons, including blood loss, lupus, or other dreaded illnesses. So he took the first step in ruling out blood loss by taking a stool sample. Note my semantics. I didn't give him one, he took it. He said to me, "It's not the high point of my day, either." At least there were no signs of blood in it. Other indicators that pointed towards Lupus included a positive Coombs' test and a high reticulocyte count. A positive Coombs' test indicates auto-immune hemolysis; the immune system prematurely destroys blood cells that it shouldn't. The high reticulocyte (immature red blood cells) count suggested that my bone marrow was over producing red blood cells in order to make up for the deficiency of mature cells. The only thing left to test was my bone marrow.
Don't you like Gloria? By testing my bone marrow, we could make sure the marrow was indeed over-producing to compensate for the anemia. So Dr. Rothberg did a bone marrow aspiration right in his office. He used some anesthetic to numb to skin over my hip bone and then shot some into the outer layer of the bone itself. Then he used a hollow needle to take a sample of my marrow. Now bone is tough stuff. He really went to town on that needle. He noticed my discomfort and asked me if I'd like to hold his nurse Gloria's hand. I declined and he said, "Don't you like Gloria?" I told him that I did indeed like Gloria; I just didn't need to hold her hand. After putting his weight into the procedure for what seemed like a rather long time, he withdrew the needle and said, "Wow. I bent the needle." Great. Then he showed Gloria and me the sample he had extracted and said, "I bet Dr. Sierocki couldn't have gotten that big of a sample." I was just thrilled to help him with his rivalry.... The pathology report showed that my bone marrow was over-producing and Dr. Rothberg was then confident that I was suffering from Auto-immune Hemolytic Anemia.
You don't NEED a Spleen My understanding of the auto-immune hemolytic process is that healthy red blood cells get inappropriately tagged for destruction. They are then filtered out by the spleen. So to prevent the red blood cells' early demise, one can have one's spleen removed. The cells get tagged, but they don't get filtered as aggressively once the spleen is gone. Dr. Rothberg was getting ready to vent my spleen... literally. In preparation for the possible splenectomy, I received the Pneumovax 23 vaccine. Spleenless people are more susceptible to Pneumonia, apparently. A CT scan of my spleen showed that it was slightly enlarged, which indicated it was working overtime. At that point, my hemoglobins were below 10 and I was feeling it. We had agreed that we'd see what the next lab results were before we made a decision about the splenectomy or changes in medication. Dr. Rothberg was also considering an increase in prednisone--from 10mg to 40 or 50mg. 1995So now what?Early 1995 After several months of steady decline, my hemoglobins rose from less than 10 to just over 12...with no -ectomies or changes in medication. Given the improvement, removing my spleen was no longer an issue. I had been telling people that if I'd had a splenectomy, I wanted to be called "Spleenless Brett." I was terribly disappointed. NOT! Dr. Rothberg was pleased with the improvement but my hemoglobins and hematocrit had not returned to normal. Rather than increase my prednisone dramatically from 10 to 40 or 50mg, he chose to split the difference and I started taking 20mg per day. Over the next few months, my immune system started behaving better -- either on its own or as a result of the extra prednisone. The anemia cleared up and I began to taper off the prednisone. Finally, I was getting out of the woods. Yeah, right.
Blind Panic Through the summer and into the fall, I tapered down the prednisone and continued to see Dr. Rothberg to monitor the anemia. I think I had gotten down to less than 10mg a day. Then one day, as I was sitting at Moe (an SGI workstation at work), I noticed that the hard drives looked odd. As I looked around, things weren't quite right. I covered my right eye and I realized that the lower half of the field of view of my left eye was medium grey. I immediately called Dr. Roberts who told me go to an ophthalmologist immediately, fearing I might have a detached retina. Right after I got off the phone with the ophthalmologist, my vision had returned to normal. Dr. Felton saw me right away and, luckily, found my retina solidly in place. The only explanation we could come up with was a migraine aura. Apparently these can happen without the migraine headache. Over the next several weeks, different parts of my vision would go grey for five to ten minutes. No headache, no sparkles, just grey. The first time it happened, it scared the poop out of me. After that, it wasn't so scary, just weird.
Gasp! As the weather started to cool, I started running a fever and had some cold symptoms. I went to see Dr. Rothberg for a scheduled follow-up and he listened to my chest and expressed surprise that I hadn't called or come in sooner. He prescribed an antibiotic for me. Amoxycillin, I think. Shortly after that, I went to see Dr. Roberts for a followup. I think I had almost finished the amoxycillin course but there was no improvement so he prescribed Biaxin. By that time, the fever had been coming and going for quite some time. I assured Jenn (at the time, my girlfriend; she's now my wife) that I was well enough to go into New York to see Beauty and the Beast on Broadway. Because it would be a late night, I slept on the fold-out couch at her parents' house in Kearny rather than driving all the way back to Princeton. About four in the morning I woke up and had difficulty breathing. When I inhaled normally, I felt like I was being stabbed in my lower right chest. Being a bit of a stoic and not wanting to inconvenience Jenn's family, I lay awake and tried to limit the depth of my breathing to avoid the pain. After everybody woke up, I called Dr. Roberts but he wasn't on for the weekend. A covering doctor returned my call. I went to the emergency room at West Hudson Hospital in Kearny where they did a chest X-ray. The X-ray didn't show very much, but they decided that I probably had pneumonia anyway and needed to be admitted and put on IV antibiotics. I was just beginning to learn that underplaying symptoms was not the way to avoid inconveniencing people.
IV Erythromycin Is Not My Friend The ER doc at West Hudson had me started on oxygen and IV Erythromycin. I am not allergic to Erythromycin, but the IV solution is fairly caustic. My veins burned half way up my arm. They gave me ice packs in a vain attempt make my arm feel better. The torture lasted a few days before I got lucky. (And when it comes to dealing with lupus, luck can be crucial.) The doctor on call who actually admitted me to West Hudson was an internist named Dr. Maria Viscuso. She happened to be married to Dr. Ronald Viscuso, a nephrologist. I don't know if she mentioned my case to him over dinner or what, but he came to see me and asked me about protein in my urine. I told him that I'd had positive stick tests on and off for quite some time. The possibility that this was a lupus flare and that I might need a kidney biopsy was raised. I was transferred to St. Barnabas Hospital and the IV antibiotics were stopped. Dr. Elliot Rosenstein, a rheumatologist, was called in and, finally, we determined that I did not have pneumonia and that my lupus was seriously flaring.
Brett the Biscut Warmer The fever continued to rage and Jenn wanted to warm biscuts on my head. Having realized that I was having a serious lupus flare, they put me on SoluMedrol (which is an IV solution of methylprednisolone). Because of the protein in the urine, they also started me on a low dose of Imuran. Over the course of a few days, the fever receded and I improved dramatically. I was released on 60mg of prednisone and 75mg of Imuran (with the expectation that the dose would be increased if I tolerated it). Because of the significant improvement, the mildness of the apparent kidney involvement, and my own trepidation, we elected to skip the kidney biopsy. When I began leaking lots of protein again in 1997, I realized I probably should have had the biopsy done when the the symptoms of lupus nephritis first appeared in 1995.
Happy Freakin' Holidays Prednisone has two faces. It's a powerful, fast-acting, inexpensive drug that has been credited with significantly improving the prognosis for people with Lupus. But high-dose steroids can also wreak havoc. The 60mg per day dose that I was on at this point wound me up and made me ravishingly hungry. A co-worker had his finger a little too close to my face and I had to warn him that if he didn't move it, it might get eaten. I was snacking constantly. After dinner, I'd have milk and cookies. Then an hour or so later, I'd have some pickles. Another hour later, it was back to the milk and cookies. Then for a late night snack, I'd down some potato chips. And just before bed, I'd have more milk and cookies. I was thinking constantly about food. I would read cook books in bed. I think I even brought one with me to the can, once. I had lost a lot of weight during the recent flare but was quickly regaining it. I started buying carrots and celery sticks so that I'd have something a little less fattening to snack on. The prednisone also made me impatient, irritable, and even a bit aggressive; such characteristics do not mix with the traffic, crowds, and inexperienced, temporary sales help that are so much a part of Christmas shopping. It was a good thing that I'm such an innately non violent person.
Decisions, Decisions Jenn and I had seriously talked about marriage during my hospital stay back in November. I wanted to give her a ring at Christmas. I found two (in two different stores) that I really liked. I couldn't make a decision to save my life. So I bought them both and let Jenn choose. Given the bumpy ride my health has given her, I probably should have let her keep both. 1996Got To Believe It's Getting BetterVery Early 1996 I had lost a lot of weight during the "Flare of '95" but thanks to my prednisone appetite, I quickly regained it. My health improved significantly, probably because of the high-dose steroids. The amount of Imuran (75mg) I was on was probably too low to do much of anything. Because of the improvement, my local rheumatologist, Dr. Roberts, had me off the Imuran fairly quickly. I also began gradually reducing the prednisone. Wedding planning began in earnest.
Youch! High doses of steroids can have a wide variety of significant side effects. I discovered one of the more obscure ones at 60 miles per hour. My left big toe cramped up. It was extremely painful and curled down all by itself. I had to pull over and clutching to downshift was no easy feat. I could not will my toe to straighten. But I *could* straighten it with my fingers without causing additional pain. In a few minutes, the cramp disappeared as quickly as it had arrived. I found out later that this was a carpopedal spasm and was probably related to the high prednisone dose.
Fast Track to Wedded Bliss We hadn't originally intended to rush the wedding, but an opportunity presented itself and we saw no good reason to wait. We had found a reception hall that we liked, but it was expensive and booked for quite some time. Of course a Sunday afternoon was slightly less expensive per person than a Saturday evening and Friday even was even less than Sunday and with a smaller minimum number of guests, too. But even Friday was still too expensive and availabiltiy was a problem. Looking at the calendar and extrapolating, I jokingly asked, "How about a Wednesday evening? Like July 3rd?" EVERYBODY we dealt with was thrilled to do it on a Wednesday. Every associated wedding service provider was available and they all offered additional discounts and/or free upgrades. And even though it was a Wednesday, to most people it was just like a Friday evening because of the Thursday holiday. So what was really an off-hand joke turned into pretty good day for wedding!
1996-1999Not yet written1996-1998 I haven't had time to go back and write up the history from about early 1996 though fall of 1998. 1999
Beautiful Fall Colors The trees are absolutely beautiful in the Princeton area right now but Fall has traditionally been difficult for me. Early in the month, I was revisited by extreme tenderness in my joints. I spoke to Dr. Kepecs about it and we increased my prednisone from 4 to 10mg for a few days followed by several days of 7.5mg. That quieted the joint pain down (the sulindac doesn't seem to be doing very much) and I will taper down about 1mg every 10 days to try to get back to 4 or 5 mg. In addition to the colors on the trees, there is also a rash on my face. And when I had my CBC done after the 9/24/1999 Cytoxan, my Red Blood Cells, Hemoglobin, and Hematocrit were all a bit low. Is the auto immune hemolytic anemia returning? Am I beginning to flare?
So far so good Well, I've reduced my prednisone from 7.5 to 7mg. Woo-hoo! Also, after Dr. Kepecs saw the rash on this site, he prescribed Elocon cream and it seems to be helping. Which is good, because I just renewed my license this morning and I'm stuck with this photo for 4 years. He and I are also going to discuss the possibility of starting Plaquenil which should help (in several months, anyway) the rash and the persisting arthralgias. My wife's birthday passed uneventfully this month which is a dramatic improvement over last year. My health last fall pretty much precluded her having a happy birthday. So far so good. With this new team of doctors, I hope to prevent a repetition of last year's catastrophe. After the last low hemoglobin, RBC, and hematocrit, I should really get my CBC repeated for peace of mind. (One of the early manifestations of my lupus was auto-immune hemolytic anemia.)
This is my brain Last Thursday, I went to Dr. J.P. Mohr, the Sciarra Professor of Clinical Neurology at New York Presbyterian Hospital's Neurological Institute. He confirmed that, contrary to popular belief, I do have a brain. Last fall, there was some concern that I was having neuropsychiatric (NP) manifestations of lupus. There had been a lumbar puncture (aka spinal tap) and a high-field MRI of my head at the time. Dr. Mohr evaluated these as well as an older MR from 1995. He felt the MR's were entirely normal and that my hippocampi were so normal that they showed almost no sign of anterior horn of the lateral ventricles (in the coronal section). His examination showed that I had normal fundi, vessels, and discs (in my eyes). And in addition to speaking easily and generating novel sentences, I made no semantic paraphasias and performed well on simple tests. Woo-hoo! He also did a transcranial Doppler on the off chance that there would be signs of flow resistance, as has happened in a few instances of multi-focal infarction. In English: There are no apparent injuries to my brain. It's healthy. And while Dr. Mohr didn't see anything to indicate NP lupus, it can't be excluded. He felt that a diagnosis of "I don't know" [what caused some of last Fall's problems] was better than a guess. Though I had hoped for something a little more concrete, I appreciated this. It's important to keep an open mind and consider all possibilities when dealing with something like lupus. As much as we all want to pin down what we're dealing with, if we don't know, it's better to treat it as such than to act on a guess.
Another Dose This past Friday, I had another dose of Cytoxan. It had been 9 weeks since the previous dose. And if the next round of blood work is favorable, we're going to space out the doses to every 12 weeks. Though I've been tolerating the Cytoxan fairly well, I will certainly be happier with the longer spacings. Overall, I have been relatively fortunate: No puking or noticeable hair loss. I just feel kind of queasy. I'm not sure I'd even really call it nausea. Taking extra prednisone the day of the treatment really seems to help. I'm not convinced the Zofran does much, though. And after a treatment, I belch a lot and end up constipated. Between the burping and the constipation-induced crankiness, I'm a joy to behold. I still felt pretty lousy on Monday (and it was a yucky day here in New Jersey), so I took another day off from work. I slept most of the morning and burped most of the afternoon. By Tuesday morning, I felt much better and today (Wednesday), I feel even better and am far more presentable. Also, my primary care doctor, Dr. Murray, keeps mentioning that he doesn't think 5mg of Vasotec is really enough to protect my kidneys. So I asked Dr. Williams, my nephrologist, if we should raise the dose. She agreed with Dr. Murray so I'll be working my way up to 10mg as I watch my blood pressure to make sure it doesn't go too low. I want to get a feel for what's normal at the current dose of 5mg before I start taking 7.5mg so I really need to start taking my BP more regularly. Just a little while ago, it was 136 over 77 with a pulse of 93 bpm. Overall, I'm pleased with how things are going. However, I have learned that I can never let my guard down. Just as I learn how to deal with the latest manifestation, something new and unexpected seems to happen. I figure that sooner or later, remission will be the only curve-ball left for lupus to throw at me.
2000
From 8 to 12 Weeks I discussed my latest lab results (from 12/20/1999) with Dr. Kepecs. Though it's still elevated, my double-stranded Anti-DNA has been fairly stable near 40 for quite some time. My C3 complement has been normal since early 1999. The C4 complement has stayed right near the lower limit of normal, sometimes a tad above, sometimes a tad below. And, aside from the flu about a week ago, I've been feeling pretty good. So my next Cytoxan dose will be 12 weeks (instead of 8 weeks) after the last one! We'll see what happens with the less frequent dosing and watch for any back-sliding in my labs. Next dose: March 3, 2000. Regarding the flu.... There are a few schools of thought on flu shots for people with lupus and/or who are on immunosuppressants. I'm going to have to sort out what to do for next flu season. When I started feeling sick, I saw my primary care doctor right away and he gave me Relenza. (5 day's worth of samples! The pharmacies around here were all sold out.) That's the stuff that you suck into your lungs. It's not really clear whether these anti-flu meds do much, but I only felt miserable for about 2 days. Then I just had minor cold symptoms. Because I'll never know how I would have felt without the Relenza, I have no way of telling whether it helped at all.
Monkey Bump I've had this monkey bump on my elbow for a few weeks now. (A monkey bump is a bump that you can't remember doing something to cause.) It's squishy. It doesn't hurt. You know that gel they use in bike seats and shoe inserts? It's like having a bit of that attached to my elbow. I went to see my primary care doctor, Dr. Murray, about it (and to have some labs done for Dr. Williams) and he instantly recognized it as an olecranon bursitis which is typically caused by trauma of some sort. (And since I could not recall any trauma, it meets the technical criteria of a monkey bump.) He didn't seem to think that my lupus had anything to do with it, but I'm going to follow up with Dr. Kepecs, my rheumatologist. Dr. Murray recommended against draining it (which is an option) because of the risk of introducing infection. He advised me to wrap it. I haven't figured out how do that effectively without having my hand go numb, though. As for the lab tests, my sed rate was normal at 12 (<=15 is normal) and my urinalysis was also normal with no red blood cells and 0-5 white blood cells. I'll be going for my next dose of Cytoxan on March 3rd and we'll do the aDNA, C3 and C4. I'll also do a 24-hour urine at Dr. William's request. She'd like to see if the higher dose of Vasotec (10mg up from 5mg) has had any effect. As long as things stay reasonably good, we'll continue with the 12 week spacing.
Burp City Excuse me. I had my 1200mg of IV Cytoxan as scheduled yesterday, so I...excuse me again...have been belching up a storm. I'm a bit queasy, but not too bad. Eating actually seems to help. We went to Subway for dinner and, because we had a coupon, I ate a whole foot-long myself and half of my wife's foot-long, too. I sure hope constipation isn't a problem again. So far so good Dr. Kepecs had a resident with him yesterday and it turns out he was in med school (a year behind) a very good friend of mine who's finishing her residency in Boston. She was actually the person who recommended Dr. Kepecs to me. Small world.... I also accepted Dr. Kepecs offer to drain my monkey bump. (He agreed that it was olecranon bursitis and thought it was worth draining.) He gave me a little bit of local anesthetic and just sucked the bursa dry with a syringe. The fluid was fairly transparent with just a hint of blood in it. He felt confident that it wasn't infected but, just to be safe, he sent it to be cultured. He also checked it under the microscope for uric acid crystals, which are a sign of gout. There weren't any, but he did show me a reference slide of uric acid crystals. This reminded me of a story about the discovery of polarizing film which I'd better verify before I repeat again.... I'll follow up with him to find out about the aDNA, C3 and C4 complements, and the fluid culture. As usual, I'll go for a CBC ten days after the Cytoxan to make sure my white count isn't perilously low.
Wait and See.
In the graph to the left (click on it to enlarge it), you can see how my labs improved when I was getting the Cytoxan every 4 weeks. And then how the aDNA jumped up when we went to 8 week spacing. This last jump bothers me a bit. But as I'm thinking about it, I'm reassuring myself a little. The labs may very well be better when we repeat them in April. The previous dose was 11 weeks after the one before that. The tick marks correspond to the dates of the lab work and a dose of Cytoxan--except for December '99: I got Cytoxan on 12/10/99 but the labs were drawn on 12/20/99. And the 12/20/99 aDNA isn't really any different from the previous three. So after this dose of Cytoxan has a chance to do its thing, my aDNA may come out much better. Even if it does, we'll still have to decide if I should continue with the 12 week spacing. So I'll just have to wait and see....
Lupus Advocacy Day
I enjoyed the trip for personal reasons, as well. I roomed with Sal, a great guy from northern New Jersey who lost his daughter to lupus. I also met Danielle and her mom, Debbie. (That's Danielle and me to the right.) Danielle saw my name tag at the orientation dinner and asked me if I was the guy with the web site. Then Kerry, another woman from NJ, made the same connection. It was really neat to actually meet people that have been to this site! It was also good to catch up with Ranit, who is a research coordinator for lupus studies at a major New York hospital. I had met her a few years ago when she spoke at a local chapter meeting. Danielle and Kerry weren't the only ones looking at my name tag. In an elevator, Bernadine (also from NJ) asked me if we were related. We worked our way up our respective family trees until we realized that we shared great-grandparents making us second cousins! So we'll probably be contributing a little blood for a genetic study, which Ranit is involved with, of course!
Another Rotten Graph
On the up side, the protein in my 4/11 24-hour Urine test was only 204mg, down from 364mg in October of 1999. This may be the result of the higher dose (10mg instead of 5mg per day) of Vasotec. So I'll be discussing all this with Dr. Kepecs and Dr. Williams very soon and we'll probably be talking about giving CellCept a try. There are no large study results about using it to treat lupus, but anecdotal reports have been positive. I'm concerned that the labs may be a harbinger of a flare, which I'd certainly like to nip in the bud. But overall, I feel good so my goal is to be careful and remain wary without driving myself crazy.
I want a new drug I saw Dr. Williams on May 5th. She found a bunch of swollen lymph nodes and I had complained about an on-again off-again low grade fever. Coupled with the increase in aDNA and decrease in complements, she expressed concern about where things were going. So we talked more about CellCept. Dr. Kepecs has used it for a few of his patients with good results and felt that it might help me, too. Dr. Williams discussed my situation with another nephrologist at Columbia who felt I was an ideal candidate for trying it. So on May 9th, I started taking 500mg two times a day. (That dose will increase to three times a day once we're sure I'm tolerating it.) Dr. Williams has used it in her transplant patients and the only complaints have been gastrointestinal. Initially, I may have been burping a bit more than normal, but nothing particularly explosive. Hopefully we'll see some improvement in the lupus.
One that won't make me sick
After eight weeks on CellCept (and almost four months after my last dose of Cytoxan), early indications are very positive. As the graph shows (click on it to enlarge it), the aDNA went from 157 to 23--a rather dramatic improvement! Dr. Kepecs has observed that the aDNA usually responds to therapy before the complement levels so hopefully those will normalize in due time. When I had a CBC done after two weeks of taking the CellCept twice a day, my white count was a little low. When I saw Dr. Kepecs, he repeated the CBC and the white count came back normal. (And at that point, I had been taking the CellCept three times day for a couple of weeks.) The morphological review showed some anomolies, however: 5% of the lymphocytes were atypical, there were occasional large platelets, and slight Toxic Granulation. According to Dr. Kepecs, the toxic granulation may be a reaction to the CellCept. (He's seen it with Cytoxan, marrow recovery from chemotherapy, etc.) And if I were recovering from a virus, that would explain all of the abnormalities. The bottom line: Don't worry. Repeat the CBC in a few weeks. I'm very encouraged by the aDNA results and I keep humming Huey Lewis to myself. CellCept may meet most of his criteria. (As for "One that don't cost too much," it fails miserably,though. It's over $4 per 500mg pill.)
Down, Up, Down
The C3 and C4 complements seem to have woken up and noticed the CellCept now, too. Both are now normal! The C4 hadn't been normal since I was getting Cytoxan every 4 weeks and the C3 jumped from just below normal to the high end of the normal range. Now I have to find out if I have to worry about too much C3 complement. That's just never been an issue before!
Welcome, Welcome, Welcome to the House of Puke (to the tune of the Bear in the Big Blue House theme) Ugh! My daughter starting throwing up on Saturday. My wife started early Monday morning. I threw up once Monday morning and switched over to diarrhea. The stomach flu seems to be vicious and widespread in the New Jersey area. I was scheduled to turn in a 24-hour urine, have some other lab work done, and get a flu shot today. I felt silly canceling my doctor's appointment because I was sick. (Actually, more because we were all sick.) What a waste of pee! I do not recommend this stomach virus.
Less Complement, More CellCept
When I saw Dr. Kepecs back in November, he mentioned a paper about CellCept out of Hong Kong. It was published in the New England Journal of Medicine in October. Though the study was small (only 42 patients, half on CellCept, half on Cytoxan), I found the results encouraging. Even though the most recent lupus activity panels (C3,C4,aDNA) have been a little squirrely, I'm still optimistic--just a bit more guardedly than I was in August. Nothing is hugely out of whack and I feel pretty good. I've had some minor inflammation in my hands and wrists, but nothing the complain about.....Oops! I just did.... The other test results have all been normal or close to it. My last 24 hour urine only had 192mg of protein. That's the lowest it's ever been! Woohoo! 2001Why no updates? July 11, 2001 Because lupus-wise, my life has been boring since the last update in December of 2000. I've gotten my prednisone dose down to 4mg/day and my labs have either improved or been reasonably stable. And I feel pretty good! My wife and I celebrated our 5th anniversary last week with dinner at the Chart House and an off-Broadway show, Tick,Tick...Boom. It was a nice night out for us....I think we need to do that more often.
Another jug of pee, what glee! Aside from a bit of a cold, I'm reasonably happy with my health. My last set of anti-DNA, C3 and C4 complements (from 9/24) was just about the same as the set from July 30th. I'd like to seem them continue to improve, though. I still get the occasional swollen finger but I was pretty excited when I got my last 24-hour urine test (from 9/25) back. There was only 128.5 mg of protein in it, which is actually within Quest Diagnostic's normal range! It's the lowest result I've ever had and I'm very pleased about that. (The worst was in December of 1997: 1573 mg)
It was very boring year Healthwise, anyway. And that's just the way I like it. 2002A little more "interesting"February 6, 2002 I saw Dr. Kepecs last week and he called to tell me about the latest lab results. The news wasn't so good. My 11/26/01 aDNA was 46.6 and my C3 and C4 complement levels were 85 (actually normal!) and 13 respectively. But my levels on 1/28/02 were 374.4 for aDNA and 54 and 5 for the respective C3 and C4 complement levels. And though I haven't felt really good since my post-Christmas cold, I wouldn't describe myself as sick. People have commented at work that it looks like I've lost a little weight, too. As silly as it may sound, this mild weight loss that people notice may be a significant predictor of my health. It seems that when these labs change significantly for the worse, it often (about 75% of the time) predicts a flare 8-10 weeks off Many doctors don't follow these labs as often and with the consistency necessary for this to be very helpful, and there's also the old mantra, "treat the patient, not the labs." But given my history (and a few other, minor signs of increased disease activity), Dr. Kepecs wants to be aggressive and pulse me with steroids. He conferred with Dr. Williams and she agreed with that plan. There's no question that there's increased serologic activity. And having missed 3 months of work in 1998 (Drs. Kepecs and Williams took over in the midst of the catastrophe of 1998 and fixed me up), I'm not a big fan of "wait-and-see." There are other options to pulse steroids, but they're not particularly attractive:
Nice to meet you.... Before I got the not-so-good news I mentioned on February 6th, I had decided to switch primary care doctors. The last one mis-diagnosed my wife with gout and took a week to return a phone call when she was still having a lot of pain. So about three weeks ago, I made an appointment with Dr. Amy Etzweiler. I figured she could take a history and we could get to know each other so that when I call with an emergency, she'll know who I am. As I said before, that was before Febrary 6th.... So in addition to taking a thorough history and examining my joints, glands, and so forth, Dr. Etzweiler spoke to Dr. Kepecs and agreed to coordinate the pulse steroids. (She's in-network, 5 minutes away, and her medical group has an infusion room on-site.) I gave her my standard flow sheet and the lupus activity graph which can seen at at My Labs which she really seemed to appreciate and absorb. I got the sense that she'll be more involved in my care than my last PCP, which is a good thing. I felt bad dumping so much on her during my first visit, but she didn't seem to mind at all.
Well, INFUSE ME. I had my first course of pulse steroids this week: 1000mg of SoluMedrol on Wednesday, Thursday, and Friday. I was able to schedule it for 4pm each day to help minimize time away from work. Because I didn't know quite what to expect, I told everybody at work not to expect me at all on Thursday and Friday. Steroids can really wind you up, so they gave me a prescription for Valium to help me sleep at night. As it turns out, I didn't take the Valium and I slept pretty well. The first night, I was up about an hour later than normal....no worse than if I drink an iced tea with dinner. And I had had an iced tea with dinner that night! I did feel a little "wired" but it wasn't bad at all. My biggest complaint was the funny taste in my mouth. Dinner tasted awful and I felt a little queasy but the problems were mild compared to the post-Cytoxan blues. Breakfast on the days following the infusions tasted almost normal and I was able to go to work. I felt a little thick headed but I mean that somewhat literally; it was more of a physical sensation and I was able to think and work as well as I normally do. Over the weekend, however, I had a bit of an energy problem. I was moderately fatigued and sleepy for most of the weekend....not what I expected at all! I had figured I'd be up early scrubbing tubs and cleaning out the garage. Oh well!
I feel like a teenager again.... Well, not quite. I don't feel young and healthy. But boy have I got the teenage acne. I've had some significant eruptions which are probably a result of the pulse steroids and/or the slightly higher daily oral dose of prednisone. (I had gone from 4mg to 15mg about a week before the first set of pulse doses and then went down to 10mg, which is what I'm taking now.) I had a follow-up visit with Dr. Etzweiler today and she prescribed Cleocin-T lotion and indicated that if it didn't help, she'd refer me to Dermatology. I also think the texture of my hair has changed. My wife noticed a difference and it feels finer and smoother to me. I had noticed a similar effect when I was taking much higher daily oral doses. Weird!
Infiltrating the Lobe I followed up with Dr. Etzweiler on the how things were going but I did have the makings of a cold. By the 15th, the cold was definitely in the chest. Time for a chest X-ray, Levaquin and cough syrup with codeine. The X-ray showed an infiltrate in the upper right lobe. This warranted delaying the next pulse steroid dose scheduled for the following week.
I'm Improving! Each successive lupus activity panel (aDNA and C3 and C4) has been been better than the previous. The pulse steroids seem to be working and with fewer side effects than a higher oral dose of steroids or Cytoxan treatments. Over this time period, I got to know the nurses in the infusion room, all of which are great. Joan, Barb, Jennifer and Lori are the primary infusion nurses and it's easy to see why patients sing their praises so often. They're right there along with the patients trying to beat the crap out of a variety of illnesses that require chemotherapy.
Bloated-Man!
Chest Pain but no 911, Please It's Friday and I've been having odd chest pain since last night. If I lean over forwards, it gets more intense, then settles down. It's not very painful, more like a dull ache. If it weren't Friday and it wasn't Memories Expo tomorrow, I'd wait until the next day.... So I call Dr. Etzweiler's office about 1pm, and of course, you say the words "Chest Pain" and they get excited. I'm not thinking heart attack, more like pericarditis. Dr. Etzweiler actually has an open appointment so I drive myself down there. When I get there, she's already scheduled an EKG and when I see her after the EKG, she's already spoken to the group's cardiologist, Dr. Costin and arranged for an echocardiogram. She listened to my heart and did not hear any signs of pericarditis. The echo is normal....while I was having it done, I realized that when Dr. Etzweiler asked if it felt like reflux and I had said "no," I really should have said that I have no idea what reflux feels like. Given the normal EKG (they also compared it to one Angelique had taken a week earlier for the LJP1082 study and faxed to them), echo and exam, Dr. Etzweiler felt the most likely cause was reflux. I agreed to stop the Vioxx and she gave me a script for Nexium. I took the Nexium that night and by the next morning I was starting to feel better. Did the Nexium really work that fast or would I have felt better the next day even if I hadn't caused all that drama? I'll never know.... I ended up restarting the Vioxx again on Thursday night, 5/9/02, because my knees were starting to bother me and Friday was opening day at Sesame Place. I feel as if there's this balance between my lupus and my medications. Everything seems to be stable if less than ideal.
Maybe I'm Not Getting Better.... Of course after five doses, the lupus activity panel went the wrong way again. I received the sixth dose of pulse steroids on 7/17/02, but Dr.Kepecs and Dr. Williams agreed that pulse Cytoxan was now the way to go. I discontinued the CellCept a few weeks before my first pulse Cytoxan (of this round of treatment). I also worked out that if I were to get the first dose on August 9, each successive dose would fall immediately after Halloween, Thanksgiving and Christmas, though one would land smack dab on my birthday.
Back on the Zac About a week ago, I told Dr. Martinson about some of my concerns, not outright depression (ie. sadness), but just an increased frustration level and general crankiness. He thought going back on Prozac prophelactically made sense. He said if I were a new patient, he wouldn't put me on it based on what I described, but given my history and the current increased lupus activity (there was increased SLE activity during my earlier neuropsychiatric problem). Though a course of anti-depressants usually runs on the order of a year, he felt that if the lupus was under control sooner than that and I was doing well, I might not need to take the Prozac for that long. Also, because I never stopped taking the Neurontin, he's comformatble reinstating the Prozac. If I were not currently on a mood stabilizer, starting an anti-depressant would be more complicated.
Last Pulse Steroids, Now What? Today is the first day of my 6th pulse steroid dose and Dr. Kepecs just happened to call with the most recent blood results. He's unhappy with the rise in aDNA and only modest improvment in the C3 and C4. He thinks a return to Cytoxan is in order, maybe as short as 3 or 4 doses. I go to see both him and Dr. Williams on 7/24 and then Dr. Etzweiler on 7/29. If Williams agrees with Kepecs, I'll set up an appointment with oncology at PMG and do the Cytoxan right at PMG under the direction of Etzweiler and a group oncologist. If I can start on Friday, 8/9 and go every four weeks, and if I go as long as six doses, I'll have one immediately after Halloween, Thanksgiving, and Christamas, though one falls right on my Birthday. I think we'll try to squeeze a trip to WDW in December. :)
My Poor, Poor, Mouth I received the same dose of Cytoxan as I had before (1200mg) but I had a vastly different reaction. I developed horrible mouth sores that I wouldn't wish on my worst enemy. I lost 20 pounds in a matter of weeks. Dr. Lee and Dr. Kepecs agreed on postponing the next dose two weeks and reducuing the dose 20% to 960mg. We also decided to wait six weeks for dose #2 so it would fall right after the trip to Disney World that we had hoped to take.
Bad Blood Work If only I knew....If I had known my double stranded anti-DNA was over 3000, we probably would have postponed our trip scheduled the following week. Of couse RDL didn't receive the blood until 10/21/02 and didn't issue a report until 10/26/02.
Disney World... ...and how it saved my life. Emily knows we're going to the airport by Grandma and Grandpa's house but Nana & Grandad are with us and she has no idea that she's going to be dining with Chef Mickey that evening. Never mind the Cinderella's Table breakfast that Jenn managed to snag a reservation for. Reservations for this particular character breakfast are so hard to get that Disney now requires a deposit to place them. While some people may question the wisdom of going on this trip, I have a few thoughts on the subject. My family needed this trip. I needed this trip. Granted, we wouldn't have gone had I known that my aDNA was so out of whack (over 3000), but my post-WDW aDNA was actually dramatically better (328) than my pre-WDW aDNA. Perhaps adrenaline and the sheer joy taking Emily to Disney World was thereapeutic to some degree. Or perhaps the two doses of Cytoxan (1200mg and 960mg) had started to work aleady. In any event, I don't think it hurt my health or delayed the recognition of the seriousness of this flare. In some ways it helped because the ultimate decision to come to see Dr. Williams was spurred by me running out of vacation and sick time. Otherwise I would have just continued on the pulse Cytoxan path until I was out of sick time and it's not clear that the pulse Cytoxan path would have worked.
Back to Work I had thought I would have enjoyed managing a contract and I had thought I'd have been pretty good at it. Neither was true and my stress level returned to high. My performance at work has been gradually declining and my fatigue level has been increasing. What to do?!? I'm so low on vacation and sick time that I have to take some of our recent vacation as unpaid.
Financial Decision I spiked a fever of 102 the previous week so Jenn & I were looking at another short paycheck. So the ultimate decision to go out on short-term disability was made the evening of Tuesday, November 19th and was primarily financial. I hadn't accomplished anything that Monday so I really couldn't put down anything other than zero hours anyway. This gave us the breathing room we needed to figure out what the hell was up with my health. Jenn insisted that I see Dr.Kepecs immediately so he could see just how sick I had become. My father came down to provide limo service. Needless to say, Dr. Kepecs saw just how sick I was. He increased my daily oral prednisone to 60mg/day (from 15mg) and we scheduled IV pulses of 1g of Solu-medrol for Monday, Tuesday, and Wednesday of Thanksgiving week with the (as previously schedule) Cytoxan for that Friday.
Fire in the Hole! I wasn't feeling too bad, but Thanksgiving was a bit exciting. Some drippings from the turkey had gotten down past the pan and caught fire. There were flames and everything. Jenn started to evacuate Emily and Jenn's dad ran for the fire extinguisher. Mrs. Lacki and I were the calmest of the bunch--we felt we should just leave the oven door closed and watch what developed. The flames died out due to lack of oxygen and we didn't create a big mess with the fire extinquisher. There was a small miracle, though. Even though the turkey had been in the oven only about half the time it should have, it was evenly cooked to temperature. Of course the side dishes were out of sync, but it sure beat the alternatives.
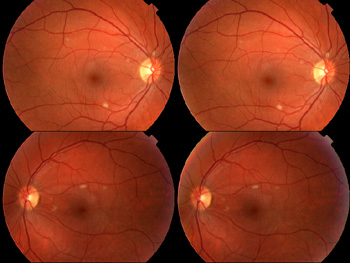
Cotton Wool Spots
For a few weeks now, I've been noticing problems with my vision. The photos on right show what Dr. Thromberg (O.D.) saw when she examined me. She explained that since this was a medical issue. I really needed to see Dr. Lui, an M.D. a week or so later. He felt this was clearly lupus retinopathy. As for treatment, we were already doing more for the systemic lupus than he would have done for the retinopathy alone.
Admission Day I'm not right. My mood is weird, I'm febrile, and I'm just plain ill. My father comes down to provide limo service and I see a doctor or two locally and end up with Dr. Williams having me admitted at New York Presbyterian. Dr. Blume is put on my case.
Double Vision I've started having double vision....or at least one and a half. My visual acuity in each eye is probably better than 20/20 but with both eyes open, I have trouble seeing.
2003Double Vision RevisitedJanuary 10, 2003 I had a quick exam with Dr. Odell, the neuro-ophthalmologist becuse of the continuning double vision. He didn't seem to think there was a neurolgical problem and that my vision should return to normal on it's own. If it doesn't, I'm to see him in a month.
Discharge Day I come home on lots of steroids (about 300mg of prednisone every other day) and oral Cytoxan (125mg). I'm better than I was but I still have a long way to go. And a lot of weight to gain back. Retinal ImprovementFebruary 6, 2003 I saw Dr. Liu again for a follow-up and he told me I was now 20/20 in both eyes. I still don't think my vision is as good as it was before I got very ill, though. There is obvious improvement in terms of the cotton wool spots on the retina images as you can see below. Some of the minor vision problems could also be side effects of some of the medications I'm taking.
2005Where has the time gone?February 1, 2005 Wow, it's been a long time since I last updated! I've gotten a few e-mails from concerned folks asking me if OK.... I actually am! In fact, that's part of the reason for the lack of updates. I got tired of eating, breathing and sleeping this disease. I'm still vigilant but not quite so militant. I just counted and realized that we've taken Emily to Disney World THREE times since the last update! (Thank you, Southwest Airlines, for super-low fares from Philadelphia to Orlando!) Things have been gradually improving and I'm almost off prednisone and Cytoxan entirely. I expect that next week Dr. Blume will tell me to stop taking the 2.5mg of prednisone and 25mg of Cytoxan that I've been taking once a week. I'll try to be better about making periodic updates if things stay wonderfully uninteresting. (If my lupus gets "exciting" again, I'll be sure to post updates.)
Now 100% immunosuppressant-free! It's official! My last dose of oral Cytoxan was March 14th, 2005! (So no more Mesnex, either.) My last dose of prednisone was February 7th, 2005 and I stopped the cortisone sometime at the end of January. The labs have held up and I've felt good to boot! This slow ween seems to have worked. I was taking very low doses of the Cytoxan (25mg) and prednisone (2.5mg) every 7 days at the end. I don't know if it was the alternate-day prednisone therapy that allowed me to get off the steroids with relative ease or what, but I'm quite pleased. (I know some people can't get below 5mg or so even if they try going in .5mg steps.....) For the next few years (up to 5, really) I'll still need stress steroid coverage if I have surgery or suffer a trauma. That's fine by me! 2009RBC's in the PeeNovember 4, 2009 I went for my semi-annual check-up at New York Presbyterian today. Lupus-wise, I'm all good: C3 & C4 complements were normal and my aDNA was just a tad above normal, which it always is, although I think it may be the lowest it has ever been. That's a big load off! I'm not sure why I was worrying the last couple of days, but I'm happy now. Four and half years of remission! Woo-hoo! The only negative was that there were some red blood cells in my urine. So I repeated the test at the doctor's today, and they'll also run a urine cytology. I'll go for a sonogram of my kidneys, too. I'm hoping for some interesting images to add to the site. (Not too interesting, mind you....) So what could this be? The concern is that it could be related to all the drugs I've done. (i.e. Cytoxan. I just like sounding cool, like a washed-up 70's rock star.) I'm not really worried about that....I'm worried that a positive cytology will mean my bladder gets a date with a little camera. Sure, they use a flexible scope these days and they've gotten better with anesthesia....but STILL! I'd better get cool images if it comes to that!
How's it look in there? So earlier this week, I got a call from my nephrologist. She had seen the repeat urine tests, the urine cytology, and the renal ultrasound report. She discussed everything with my rheumatologist and they felt that, between the little bit of nephrocalcinosis seen in the ultrasound and the RBC's in the urine, I should see a urologist and have a cystoscopy. So Tuesday morning I call their preferred urologist and the soonest I can get an appointment is January 11th. There's nothing about my situation that seems terribly urgent, but I had a couple of other things to tell my nephrologist, so I called her and asked her if January was soon enough or if I should make other arrangements. She said, "Let me call you back." Ten minutes later, I get a call: "When you hang up, call the urologist. They'll give you an appointment for 9am tomorrow." So this morning, I get up early, make good time on Route 1, get tied up on the 1/2 mile of Route 18, and haul ass on the Turnpike. So I was expecting this morning's appointment to just be an office visit and that I'd have to schedule and come back for the actual cystoscopy. But, as luck would have it, the doctor was able to do the procedure a couple of hours later. I guess that was good luck.... Guys, let me tell you, this procedure is a treat. My urologist is a little old school (no complaints - old school medicine got me into remission), so I don't have any cool images. As he was peering around in there, he noted that there were changes to the bladder wall that are expected after Cytoxan therapy. The blood vessels are closer to the surface and more pronounced. There were no signs of malignancy and he didn't have to biopsy anything. So it sounds like everything is OK on the bladder side of things. Of course there are still the kidneys to consider. I had a renal ultrasound last week and the urologist agreed with the radiologist that there are signs of nephrocalcinosis. These small calcium deposits aren't cause for any great concern at this point. They probably developed during my treatment with high-dose steroids and will not progress now that I'm not on any steroids at all anymore. He was going to discuss everything with my nephrologist and rheumatologist and felt they'd probably come to an agreement that I should have a CAT scan of my kidneys. The CAT scan is much better for seeing this than an ultrasound and it would give is a baseline in case we need to look for changes in the future. Overall, I'm pleased. Getting my SLE into remission only to end up with bladder cancer from the Cytoxan therapy that did it would have kinda sucked.
2014I Like Pi3/14 I've gotten a few worried emails and messages because the last update was so long ago so I thought I should post a quick "All is (still) well!" update. I'm healthy, I'm working hard at the same job I've had since I graduated college, and the rest of the family is well, too. So what's with Pi? I didn't make the connection between the date and Pi Day at the time, but I swallowed my last dose of Cytoxan nine years ago today. I had discontinued Prednisone the month before. I continue to take enalapril and simvastain to mitigate coronary heart disease risks. My my primary care doctor noted that my Vitamin D was a little low when I had my physical earlier this year so I added some extra Vitamin D.
So I have not had any immunosuppressants or Disease
Modifying Anti-Rheumatic Drugs since Pi Day 2005 so that's one more reason to like Pi.
And a few years ago, I realized that my phone extension at work wasn't three one four - it was Pi!
|

 Yesterday
afternoon, I drove down to Washington, DC to join about a dozen other
people from the NJ chapter of the LFA. People from all over the
country converged to meet with their senators and representatives (or
at least members of their staffs) to urge them to support the Lupus
Research and Care Amendments. Both the House and Senate bills would
add about $30 million to the National Institute of Health's lupus
research budget. I learned a lot about how Congress works and while
the bills have many supporters from NJ (my home state), I don't think
the hold outs will be changing their minds. Nationally, the bills
enjoy good support and from what I heard before I left DC, three
additional senators became interested in cosponsoring the Senate bill
as a result of our efforts.
Yesterday
afternoon, I drove down to Washington, DC to join about a dozen other
people from the NJ chapter of the LFA. People from all over the
country converged to meet with their senators and representatives (or
at least members of their staffs) to urge them to support the Lupus
Research and Care Amendments. Both the House and Senate bills would
add about $30 million to the National Institute of Health's lupus
research budget. I learned a lot about how Congress works and while
the bills have many supporters from NJ (my home state), I don't think
the hold outs will be changing their minds. Nationally, the bills
enjoy good support and from what I heard before I left DC, three
additional senators became interested in cosponsoring the Senate bill
as a result of our efforts.